ORANGE, Calif. (March 24, 2023) — Medi-Cal members will soon be required to verify their eligibility for the program. The annual renewal process, which was suspended during the pandemic, could result in thousands of people losing their health care coverage. The state estimates that up to 20% of members could lose coverage.
Medi-Cal members have not been required to verify their eligibility for the program since the renewal process was suspended during the public health emergency. But starting April 1, the process resumes and will continue for 14 months. During that time, members will need to respond to requests from the County of Orange Social Services Agency (SSA) for renewal information, such as income and family status, to keep their Medi-Cal. According to local estimates, 10% to 15% of members could lose coverage. To limit this impact, CalOptima Health, Orange County’s Medi-Cal plan, is investing $6 million to raise awareness and hire community-based staff to help our more than 970,000 members.
“Imagine going to your doctor appointment and finding that you’re not covered,” said Michael Hunn, CEO of CalOptima Health. “What if you need medication and now can’t get it — it’s a life-altering issue. We are responsible for supporting the health of more than one in four Orange County residents, and we need to take the lead in educating our community and members who don’t realize they need to renew their health benefits — or risk losing them.”
SSA will first try to renew Medi-Cal members automatically with information available in its systems. If automatic renewal isn’t possible, SSA will mail a renewal form to members’ homes in a special yellow envelope. Renewal forms will be sent 60 days before members’ current renewal month in their case records. Members will get multiple reminders to complete their renewal forms. However, mailings can pose a challenge because members’ addresses may have changed, or they could be experiencing homelessness and lack an address to receive the form.
The CalOptima Health funding will support hiring up to 100 enrollment navigators in community health centers across Orange County to assist members in completing this important process. The agency also plans to launch a robust, multichannel communications program that includes phone calls, texting, flyers, community events and other tactics to raise awareness.
CalOptima Health is urging Medi-Cal members to take action:
- Update your contact information (phone, address and email) with SSA (1-800-281-9799).
- Check your online Medi-Cal account at MyBenefitsCalWIN.org.
- Check your mail for a special yellow envelope with your renewal form. It will be sent 60 days before your current renewal month in your case record.
- Complete and return your renewal form within 60 days to keep your coverage.
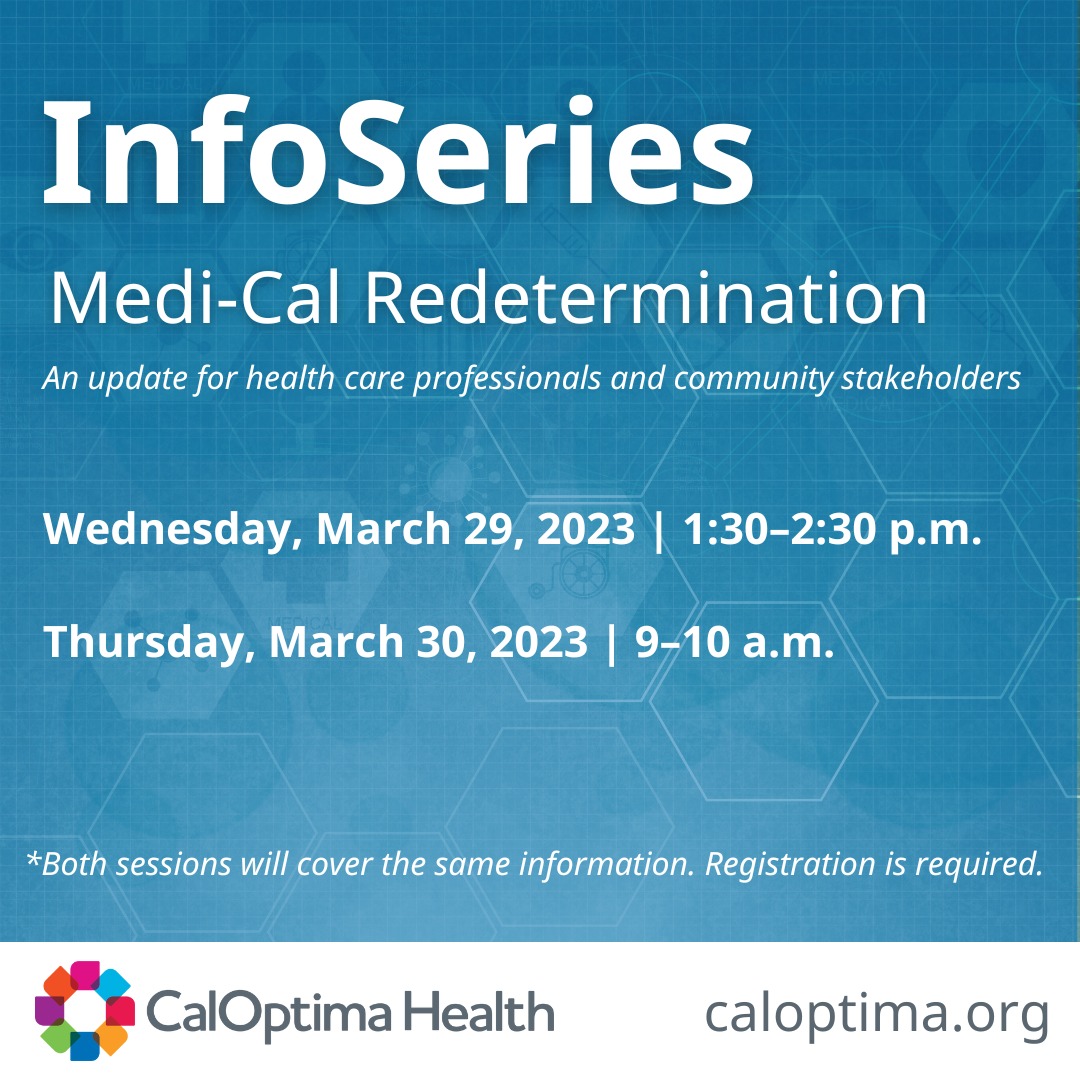
Learn about the Medi-Cal Renewal Process at CalOptima Health’s next InfoSeries on Wednesday, March 29, 1:30–2:30 p.m. and Thursday, March 30, 9–10 a.m.
The session will cover:
- The Medi-Cal Redetermination timeline and what members can expect
- How members can report a change
- Important resources
Register by Tuesday, March 28.
Register for Wednesday, March 29 at: https://bit.ly/caloptimahealthinfoseries0329
Register for Thursday, March 30 at: https://bit.ly/caloptimahealthinfoseries0330